Ascites Facts
- Ascites refers to abnormal accumulation fluid in the abdominal (peritoneal)
cavity.
- The most common cause of ascites is cirrhosis of the liver.
- Treatment of ascites depends on its underlying cause.

What is ascites?
Ascites is the accumulation of fluid (usually serous
fluid which is a pale yellow and clear fluid) in the abdominal (peritoneal) cavity. The
abdominal cavity is located below the chest cavity, separated from it by the
diaphragm.
Ascitic fluid can have many sources such as liver disease,
cancers, congestive heart failure, or kidney failure.
What causes ascites?
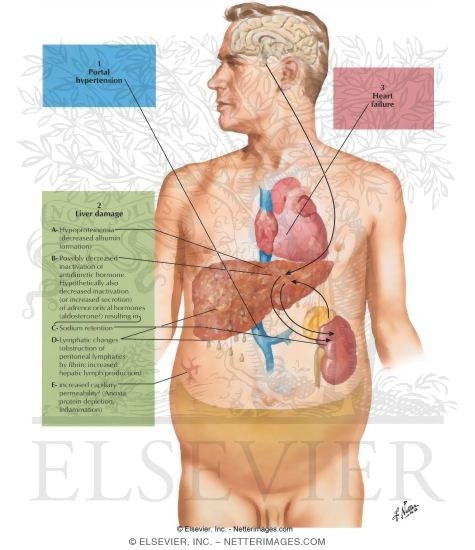
The most common cause of ascites is advanced liver
disease or cirrhosis. Approximately 85% of the ascites cases are thought to be
due to cirrhosis. Although the exact mechanism of ascites development is not
completely understood, most theories suggest
portal hypertension (increased
pressure in the liver blood flow) as the main contributor. The basic principle
is similar to the formation of edema elsewhere in the body due to an imbalance
of pressure between inside the circulation (high pressure system) and outside, in this case, the
abdominal cavity (low pressure space). The increase in portal blood pressure and
decrease in albumin (a protein that is carried in the blood) may be responsible
in forming the pressure gradient and resulting in abdominal ascites.
Other factors that may contribute to ascites are salt and water retention.
The circulating blood volume may be perceived low by the sensors in the kidneys
as the formation of ascites may deplete some volume from the blood. This signals
the kidneys to reabsorb more salt and water to compensate for the volume loss.
Some other causes of ascites related to increased pressure gradient are
congestive heart failure and advanced kidney failure due to generalized
retention of fluid in the body.
In rare cases, increased pressure in the portal system
can be caused by internal or external obstruction of the portal vessel, resulting
in portal hypertension without cirrhosis. Examples of this can be a mass (or
tumor) pressing on the portal vessels from inside the abdominal cavity or
blood
clot formation in the portal vessel obstructing the normal flow and increasing
the pressure in the vessel (for example, the Budd-Chiari syndrome).
Acites can also manifest as a result of cancers, called malignant ascites.
These types of ascites are typically manifestations of advanced cancers of the
organs in the abdominal cavity, such as, colon cancer, pancreatic cancer,
stomach cancer, breast cancer,
lymphoma, lung cancer, or ovarian cancer.
Pancreatic ascites can be seen in people with chronic
(long standing) pancreatitis or inflammation of
the pancreas. The most common cause of chronic
pancreatitis is prolonged alcohol abuse.
Pancreatic ascites can also be caused by acute pancreatitis as well as trauma to the pancreas.